Day 3 :
- Case Study on Cardiology | Research on Cardiology | Biomarkers and Enzymes for Heart Disease | Obesity and Heart | Cardiac Regeneration and Repair
Location: London, UK

Chair
Annamaria Vianello
Gabriele Monasterio Foundation, Italy
Session Introduction
Samer Ellahham
Sheikh Khalifa Medical City, UAE & Cleveland Clinic, USA
Title: The importance of multidisciplinary approach
Time : 09:30-10:00

Biography:
Samer Ellahham has served as Chief Quality Officer for Sheikh Khalifa Medical City, since 2009. In his role, he has led the development of a quality and safety program that has been highly successful and visible and has been recognized internationally by a number of awards. As Chief Quality Officer and Global Leader, he has focus on “Ensuring that that implementation of this best practices leads to breakthrough improvements in clinical quality and patient safety”. He is the recipient of the Quality Leadership Award from the Global Awards for Excellence in Quality and Leadership and the Business Leadership Excellence Award from the World Leadership Congress. He was nominated in 2015 for SafeCare magazine Person of the Year. He is Certified Professional in Healthcare Quality (CPHQ). He is a recognized leader in quality, safety, and the use of robust performance improvement in improving healthcare delivery.
Abstract:
In most countries worldwide, the number of patients with chronic heart failure (HF) is growing with 1-3% of the adult population suffering from this syndrome, rising to about 10% in the very elderly. In the near future, a large part of the worldwide population will suffer from heart failure and society will be faced with the consequences. On average, one in five patients is readmitted within 12 months, making heart failure one of the most common causes of hospitalization in people over 65 years of age. A multidisciplinary team approach involving several professionals with their own expertise is important in attaining an optimal effect. Physicians, nurses and other health care professionals are keys ensuring the delivery of evidence based care. Markers of clinical (in) stability, psychosocial risk factors, and issues related to patient mobility might be important indicators to determine which inter-professional service might be most effective for which patient. Current HF guidelines recommend that HF patients are enrolled in a multidisciplinary-care management program to reduce the risk of HF hospitalization. A multidisciplinary approach to HF may reduce costs, decrease length of stay, curtail readmissions, improve compliance and reduce mortality. An important limitation, however, is the substantial heterogeneity in both the terms of the models of care and the interventions offered, including: clinic or community-based systems of care, remote management and enhanced patient self-care. Conventional trials that randomize individual patients may not be the best way to test the effect of a service; novel approaches, such as the cluster randomized controlled trial, may be superior. It is unlikely that any one approach is optimal. The best form of care might seek to compensate for the weaknesses of each approach by exploiting their strengths. A strong HF cardiology lead, supported by primary care physicians, nurse specialists and pharmacists in the hospital and community with the ability to offer patients remote support might offer the best service. Key to the success of multidisciplinary HF programs may be the coordination of care along the spectrum of severity of HF and throughout the chain-of-care delivered by the various services within the healthcare system. Further research is warranted to identify the most efficacious multidisciplinary approaches to HF.
Learning Objectives: Objectives are to: Define multidisciplinary approach to HF; examine the literature role and recommendations of multidisciplinary in HF and; identify barriers to optimal models of multidisciplinary approach to HF.
Annamaria Vianello
Gabriele Monasterio Foundation, Italy
Title: A case of misdiagnosed cardiomyopathy with rising plasma MMP9 long before sudden cardiac arrest
Time : 10:00-10:30

Biography:
Annamaria Vianello completed her Graduation at Medical School, Pisa University where she obtained Specialization both in Internal Medicine and in General Medicine. She completed her PhD in Medical Physiopathology and Pharmacology and in Normal and Pathological Morphology of Cells and Tissues; a second-level Short Specialization Degree in Clinical Pharmacological Research and; second-level Short Specialization Degree in Hypertrophic Cardiomyopathies at Pavia University. She worked as Fellow in Department of Internal Medicine and Sport Medicine, Pisa University. Her research interests include Athlete’s Heart Remodeling, Failing Heart Remodeling and Cardio-Renal Remodeling. She is currently coordinating a Tele-Health Project for out-of-hospital care of chronic heart failure. She is an Author of original papers dealing with the clinical role of circulating and tissue profiles of inflammatory biomarkers, MMPs and TIMPs in different models of heart remodeling such as Athlete’s Heart, Valvular Heart Disease, Cardio-Renal Failure and Chronic Heart Failure.
Abstract:
Introduction: Out-of-hospital cardiac arrest in the absence of structural heart disease is rare and can be due to subclinical cardiomyopathy or primary electrical disorders. Adverse collagen remodeling may occur in cardiac arrest patients; MMP-9 is proven to help risk stratification.
Clinical Case Description: In 2005, R.R, a 35 year old metal-worker, surprisingly began to show high values of MMP9. TIMPs, MMP2, NT-pro-BNP and all the other laboratory tests, abdominal echography, electrocardiogram and echocardiography were within the reference range. 10 years later, R.R suddenly collapsed at home; his wife promptly began a successful cardiac massage, supported by territorial tele-emergency network. R.R was admitted to the intensive unit with frequent ventricular extrasystoles, left ventricular dysfunction. Medical history of his family includes sudden death of two paternal uncles; mother with Takotsubo syndrome. Unremarkable clinical examination and electrocardiogram showed no biochemical evidence of acute myocardial infarction; CRP elevation. Un-obstructed coronary arteries on coronary were revealed in angiography. Chest X-ray showed mild interstitial fibrosis. There were no signs of arrhythmogenic cardiomyopathy on Cardio-NMR.
Discharge Diagnosis: Discharge diagnosis was: “Resuscitated cardiac arrest, in subject without evidence of structural heart disease, treated with ICD bicameral system”.
Reviewing Clinical Information & Diagnosis: Familial histories of sudden death, mild endocardial irregularities, left ventricle enlargement, reduced ejection fraction, low EKG voltage are suggestive of familial cardiomyopathy. Welding, chest X-ray fibrosis, RCP is suggestive of welder’s lung. Then, reformulated diagnosis: Resuscitated cardiac arrest in sub-clinical familial cardiomyopathy, chronically subjected to professional cardio-toxic damage.
Conclusions & Implications for Clinical Practice: R.R lethal arrhythmia was firstly considered as “idiopathic” in nature, since process laboratory and radiology testing were not analyzed properly. Interestingly, long before cardiac arrest, MMP9 had begun to rise, announcing a cardio-pulmonary adverse remodeling. The case of R.R teaches us that early biomarkers such as MMP9, correct and timely diagnosis, tele-medicine and emergency services network could really save lives of patients at high risk of sudden death.
Image:
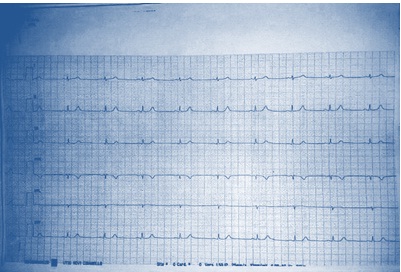
Figure 1: Low EKG voltage on peripheral leads
References:
1. Flevari P, Theodorakis G, Leftheriotis D, Kroupis C, Kolokathis F, Dima K, Anastasiou-Nana M, Kremastinos D (2012) Serum markers of deranged myocardial collagen turnover: their relation to malignant ventricular arrhythmias in cardioverter-defibrillator recipients with heart failure. Am Heart J 164 (4):530-537.
2.Turkdogan KA, Zorlu A, Guven FM, Ekinozu I, Eryigit U, Yilmaz MB (2012) Usefulness of admission matrix metalloproteinase 9 as a predictor of early mortality after cardiopulmonary resuscitation in cardiac arrest patients. Am J Emerg Med 30(9): 1804-1809.
3. Hästbacka J, Tiainen M, Hynninen M, Kolho E, Tervahartiala T, Sorsa T, Lauhio A, Pettilä V (2012) Serum matrix metalloproteinases in patients resuscitated from cardiac arrest. The association with therapeutic hypoyhermia. Resuscitation 83(2): 197-201.
4.Fang AC, Cassidy A, Christiani DC (2010) Systematic Review of Occupational Exposure to Particulate Matter and Cardiovascular Disease. Int J Environ Res Public health 7: 1773-1806.
5.Schiff GD, Hasan O, Kim S, Abrams R, Cosby K, Lambert BL, Elstein AS, Hasler S, Kabongo ML, Krosnjar N, Odwazny R, Wisniewski MF, McNutt RA (2009) Diagnostic error in medicine: analysis of 583 Physician-Reported Errors. Arch Inter Med 169(20): 1881-1887.
Prashant Tarakant Upasani
Metro Hospital & Heart Institute, India
Title: Advances in management of heart failure with emphasis on Angiotensin receptor neprilysin inhibitor (ARNI)
Time : 10:45:11:15

Biography:
Prashant Tarakant Upasani completed his DM (Cardiology) at All India Institute of Medical Sciences, New Delhi in May 1994. After completing his DM (Cardiology), he worked as Associate Consultant Cardiologist at Apollo Hospitals, Chennai and Indraprastha Apollo Hospitals, New Delhi. He is presently working at Metro Heart Institute, Noida as Senior Consultant Interventional Cardiologist. He is actively involved in all diagnostic and therapeutic interventional procedures. He was awarded Fellowship of College of Chest Physicians in the field of Pediatric Cardiology. In December 2012, he was conferred with Fellowship of Cardio-logical Society of India. He has 99 publications both in national and international journals including text books on cardiology. He has presented more than 80 papers in various national and international conferences. He is also the Coordinator of DNB Cardiology program at Metro Hospital, Noida.
Abstract:
Heart failure (HF) is an increasingly common syndrome associated with high mortality and economic burden. A range of terms has been used to describe HF viz. chronic HF (CHF), acute HF (AHF), HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF). Pathophysiology of HFrEF is complex. Landmark trails in patient with HFrEF include SOLVD-T, CIBIS-II, CHARM-Alternative and CHARM-Added, SHIFT, EMPHASISHF and PARADIGM-HF. Natriuretic peptides (NPs) are a group of hormones that have potent effects on sodium and fluid balance. Neprilysin is a zinc-dependent metallopeptidase that catalyses the degradation of various peptides. Inhibition of neprilysin increases bioavailability of NPs, bradykinin, and substance P, resulting in natriuretic, vasodilatory and anti-proliferative effects. LCZ696 is useful not only for the treatment of HF but also likely to be a useful antihypertensive drug. LCZ696 is a novel drug that comprises sacubitril (AHU377) and valsartan in a 1:1 molar ratio. It simultaneously inhibits neprilysin and blocks AT1 receptors. PARADIGM-HF is the first study to test the efficacy of LCZ696 on morbidity and mortality in patients with HFrEF. The trail was stopped early, according to pre-specified rules, after a median follow-up of 27 months, because the boundary for an overwhelming benefit with LCZ696 had been crossed. LCZ696 was associated with a significantly lower death from cardiovascular causes or first hospitalization (taken together-20% or separately 20-21%). Secondary endpoint viz. death from any cause, showed a 16% reduction (p<0.001). The superiority of LCZ696 over enalapril was not accompanied by important safety concerns. The LCZ696 group had a higher proportion of patients with non-serious angioedema, but not associated with an increase in serious angioedema.
Vladimir Ermoshkin
Russian New University, Russia
Title: The new theory of heart failure
Time : 11:15-11:45

Biography:
Vladimir Ermoshkin completed his Graduation in Physics department at Moscow State University in 1978. He has worked at Russian New University (RosNOU) as Physicist. He has published 10 articles on Cardiology in prominent magazines (Russian and English).
Abstract:
Aim:C делана попытка нового анализа м еханизм а An attempt to study the mechanism of heart failure.
Method: Information search in the literature, participate in conferences, discussions with Russian leading cardiologists.
Result: Having heart failure means that for some reason your heart is not pumping blood around the body as well as it used to. Heart failure can be a major manifestation of virtually all diseases of the heart, including coronary atherosclerosis, myocardial infarction, acquired valvular disease, congenital heart disease, arrhythmias and cardiomyopathy. Populationâ€based echocardiographic studies have demonstrated that more than 50% of participants with left ventricular systolic dysfunction (generally defined as LVEF <35–40%) have no symptoms or signs of heart failure. How to interpret this data? How the heart can pump insufficient blood to one person and sufficient amount of blood to another? Where is the logic? The reason according to my theory of CVD is that, near liver, arteriovenous anastomoses (AVA) or cascade AVA opens for longer time than optimal. Veins overflow begin mechano-induced arrhythmia. Opened AVA lead to stagnation of blood in the area of small pelvis and ankle/feet. The other reasons are stasis of microcirculations, weight gain, varicose veins, endometriosis, prostatitis, hemorrhoids, thrombosis, and cancer. The development of these diseases is accompanied in most cases with heart failure.
Conclusions: It is necessary to correct the glaring errors in cardiology which are existing from past 50-100 years. It is necessary to develop pulse wave suppressors and artificial anastomosis with an adjustable diameter hole.
1. British Heart Foundation is a registered Charity No. 225971. Internet resource. https://www.bhf.org.uk/heart-health/conditions/heart-failure
2. «ÐÐПЦССХ им. Ð.Ð. Бакулева» Минздрава РоÑÑии. Internet resource. http://www.bakulev.ru/cyclo/detail.php?ID=39219
3. Arend Mosterd, Arno W Hoes Clinical epidemiology of heart failure Journal List Heart v.93(9); 2007 Sep https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1955040/
4. Ermoshkin VI. New theory of arrhythmia. Conceptual substantiation of arrhythmia mechanisms. Cardiometry; Issue 8; May 2016; p.6–17; doi:10.12710/cardiometry.2016.8.617.
5. Ermoshkin VI. A New Theory of Certain Cardiovascular Diseases. EC Cardiology, Volume 2 Issue 5 November 2016 https://www.ecronicon.com/eccy/pdf/ECCY-02-000034.pdf
6. Ermoshkin V (2016) Pathological Role of the "Invisible" Anastomoses. J Bioengineer & Biomedical Sci 6: 209. doi: 10.4172/2155-9538.1000209 http://www.omicsonline.org/open-access/pathological-role-of-the-invisible-anastomoses-2155-9538-1000209.pdf
7. Ermoshkin VI. Heart transplantation mysteriously eliminates arrhythmia. Cardiometry; Issue 8; May 2016; p.18–21; doi:10.12710/cardiometry.2016.8.1821.
8. Ermoshkin VI. The mechanism of bronchial asthma. Why do the most serious asthma attacks occur at night? EC Cardiology, Volume 2 Issue 4 November 2016 https://www.ecronicon.com/eccy/pdf/ECCY-02-000030.pdf
9. Ermoshkin VI. Proceedings of the International Conference on arrhythmia. [Abstract] Australia. Brisbane. Arrhythmia-2016, July 14-15, 2016, http://arrhythmias.conferenceseries.com/scientific-program/ (Day 1, 16:45-17: 00).
Rhodaline Yayra Odoi
V.N. Karazin National University, Ukraine
Title: Obesity and the heart: Obesity management
Time : 11:45-12:15

Biography:
Rhodaline Yayra Odoi is a second-year Medical student at V.N. Karazin National University, Ukraine where she is currently pursuing General Medicine. She is looking forward to specialize in Pediatrics/Gynecology and Obstetrics after medical school. She has previously volunteered at Tema General Hospital (Tema-Ghana), Korle-Bu Teaching Hospital (Accra-Ghana), where she worked at the Pediatrics and Gynecology and Obstetrics department. She is looking forward to work with Hamad General hospital (Doha, Qatar).
Abstract:
Statement of the Problem: Obesity which is excess fatty weight is one of the most predominant cardiovascular risk factor. The association between obesity and cardiovascular disease is complex and not limited to the standard risk factors like hypertension, dyslipidemia, and type 2 diabetes mellitus. Recent years researches have shown that obesity causes most cardiovascular diseases through mechanisms like subclinical inflammation, endothelial dysfunction, increased sympathetic tone, atherogenic lipid profiles, enhanced thrombogenic factors, and also through obstructive sleep apnea. The purpose of this study is to create awareness of obesity, its bad outcome and to awaken us on the lifestyle we live.
Methodological & Theoretical Orientation: Based on my research done in Ghana, people with issues of obesity have cardiovascular disease.
Findings: Several studies have shown association between obesity and prognosis among those with coronary disease and heart failure, this may be due to limitations of ways we define obesity. There are numerous data suggesting that measuring central obesity or total body fat content might be more appropriate than using the body mass index method alone.
Conclusion: The management of obesity is challenging and studies using lifestyle modification alone or with pharmacologic agents generally have limited success and high levels of weight regain. Bariatric surgery has proven to be an effective and safe way to induce and maintain significant weight loss but its limited to those with medically complicated obesity or people who are severely obese therefore urging imminent doctors and medical practitioners to thoroughly educate their patients who are obese or yet to get obese on the bad effect of obesity and also encourage them to exercise regularly which may reduce their weight and also help boost their metabolic activities hence keeping them healthy.
Image:
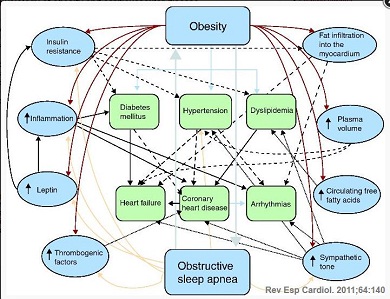
Figure 1: Pathophysiology of obesity and cardiovascular disease.
References:
1. acobellis G, Leonetti F. Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab. 2005;90:6300-2.
2. Catenacci VA, Hill JO, Wyatt H.R. The obesity epidemic. Clin Chest Med. 2009;30:415-44.
3. OECD Press Release 2010: Health: OECD says government must fight fat. Available at: http://www.oecd.org/document/35/0,3343,en_21571361 _44315115_46064099_1_1_1_1,00.html.
4. Poirier P. Cardiologists and abdominal obesity: lost in translation? Heart. 2009;95:1033-5.
5. Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881-7.
Umme Habiba Ferdaushi
National Institute of Cardiovascular Diseases (NICVD), Bangladesh
Title: Short term outcome of cardiac resynchronization therapy on functional recovery of patients with congestive heart failure in Bangladeshi population
Time : 12:15-12:45

Biography:
Umme Habiba Ferdaushi has completed her MBBS at Shere Bangla Medical College, Barisal, Bangladesh and fellowship in Cardiology at Bangladesh College of Physicians and Surgeons (BCPS), Bangladesh. She works at National Institute of Cardiovascular Diseases (NICVD), a tertiary level cardiovascular institute. She has published three papers in reputed journals.
Abstract:
Background & Aim: Cardiac resynchronization therapy (CRT) reduces symptoms and improves left ventricular function in patients with heart failure due to left ventricular systolic dysfunction and cardiac dyssynchrony. We analyzed the clinical and echocardiographic outcome of CRT in heart failure patients.
Methods: A total 35 heart failure patients were included in this prospective observational study, conducted from Feb 2015–Feb 2016 in the cardiology department of NICVD, Dhaka. Demographic profile, clinical data and investigations including coronary angiogram were done. Patients underwent CRT-P (BiV pacemaker) or CRT-D (defibrillator) and were followed up. Clinical, electrocardiographic and echocardiographic study were performed before and three months after CRT implantation.
Results: After three months of BiV pacing, New York Heart Association functional class improved from 3.3±0.44 to 1.7±0.6 (p<0.001). Left ventricular end diastolic diameter was reduced from 67.9±5.2 to 61.9±5.9 mm (p<0.001) and left ventricular end systolic diameter was reduced from 56.4±6.5 to 50.5±7.2 mm (p<0.001). Ejection fraction was significantly increased after three months from 27.5±4.3% to 38.8±6.7%, (p<0.001).The average grade of mitral regurgitation was decreased from 1.49±0.65 to 0.43±0.61 (p<0.001). The number of hospitalization was also significantly reduced from 2.51±1.44 to 0.11±0.32 (p<0.001). Among the study patients, 71.4% patient was responders, 17.1% super responders and 11.4% non-responders.
Conclusions: Although the study was performed on a small number of patients, it can be considered that CRT had favorable hemodynamic and clinical results and reduced the need for hospitalization in our heart failure patients.
Vladimir Ermoshkin
Russian New University, Russia
Title: Problems heart failure. Unexpected outcome
Time : 12:45-13:15

Biography:
Vladimir Ermoshkin completed his Graduation in Physics department at Moscow State University in 1978. He has worked at Russian New University (RosNOU) as Physicist. He has published 10 articles on Cardiology in prominent magazines (Russian and English).
Abstract:
Goal.
C делана попытка нового анализа м еханизм аAn attempt to study heart failure.
Methods.
An examination of the literature, participation in conferences, and discussions with Russian leading cardiologists.
Results.
Heart failure (HF) can be chronic (CHF) or acute (AHF). This terminology was in the 12th Congress of Physicians in 1935, more than 80 years ago. Up until now, the disease has been considered incurable and with an unknown cause, or with unknown etiology.
With current clinical position, CHF is a complex disorder with specific symptoms (dyspnea, fatigue, decreased physical activity, edema, heart rhythm and palpitations al.), which are related to inadequate perfusion of organs and tissues at rest or during exercise. Another characteristic feature of chronic heart failure is fluid retention in the body. Most often, edema begins in the lower extremities, pelvic organs and gradually rise above the body up to the heart and lungs.
Currently, the primary mechanism HF is considered the deterioration of the heart's ability to fill or empty the chambers due to damage to the myocardium, including heart attacks while with concomitant imbalance neurohormonal systems. As a rule, HF ejection fraction is reduced to 30-45%, with the required fraction of 50-65%.
The treatment of heart failure is ineffective. There is a high death rate from heart failure after diagnosis. Symptomatic heart failure occurs in 1.8-2.0% of people. Among people older than 65 years, the frequency of occurrence of heart failure is 6-10%. Further, after heart failure, the five-year survival of patients with heart failure less than 50% and the risk of sudden death in CHF is 5 times higher than in the general population.
Over the past few decades thousands of articles have been written listing the following causes: myocardial infarction, cardiac ischemia, atherosclerosis, high blood pressure (BP), disease of the heart valves, inflammatory and non-inflammatory disease of the myocardium, congenital heart defects, lung disease, alcohol abuse, drug reception, addiction to tobacco.
Thus, HF is widespread, its mechanism is unknown, the treatment of symptomatic, effective treatment of heart failure has not been found, and there is a high mortality rate.
The main conclusion of the interim etiology HF: heart failure can be a major manifestation of virtually all heart disease [1].
Heart failure necessarily occurs following a heart attack, but there are instances of heart failure where no heart attack occurred.
The new theory of cardiovascular disease is based on the fact that the arterial and venous pools may periodically be linked large anastomoses (natural shunts) [2,3,4,5,6]. In normal conditions, arteriovenous anastomoses (AVA) are closed, but during periods of increased physical and psychological stress due to increased blood pressure, they can open. The most common pathological role extended AVA manifests in the liver area. This leads to a reset of the arterial blood directly into veins. Because of this, some groups of working cells are left without sufficient food. Under certain conditions, the AVA may be open too long. As a result, blood high pressure penetrates into the venous bed and gradually fills it. Usually first affecting the liver and portal vein.
Further, high blood pressure occurs not only in the right atrium area, but throughout the vena cava, and extending downwards to the small veins. Much depends on the diameter and network location of the veins, the location of the AVA (one AVA or cascade), lifestyle, and the prevailing human posture.
Of course, a substantial pressure increase in small venules and veins occurs over a long period. In the first stage, venous valves counteract the pathological process, but after some time the venous valves begin to break down. This is due to the necessary counteraction of the total pressure of 60-70 mm Hg and above. The total pressure consists of the diastolic blood pressure and the hydrostatic pressure of the liquid column located above the valve. Due to the lack of pressure difference between arterioles and venules capillary circulation slows in some organs, or even stops. Lymph also stagnates.
In my opinion, obstacles in the form of a blood clot, tumor emboli do not raise the pressure in the veins near the venules, but add additional pressure transmitted through the veins of the confluence zone of large anastomoses [6]. Over time, because of the permeability of vascular veins occur swelling of tissues, varicose veins, venous thrombosis. Cardiology has made a mistake by confusing the cause and effect. If proper prevention is not provided, the process of the disease is enhanced, and further diseases in the small pelvis, lower limbs, and others, including some types of cancer will occur.
Yes, it is, of cancer. There are studies which have shown that the average time of the first heart attack to cancer is equal to only 2.8 years [7]. Another study shows 70% increase in the risk of cancer in patients for three years after a diagnosis of heart failure [8]. Thus, the incidence of heart failure and cancer rigidly connected and this connection is probably due to the stagnation of blood in the veins due to open AVA!
Thus, according to the new theory, the majority of cardiovascular diseases occur due to malfunction of the AVA, due to venous plethora. Extras: because pulse waves running through a crowded vena cava, with mechanical and electrical excitation arrhythmic CMC [2, 9].
Thus, in my opinion, the following provisions must be corrected in cardiology.
1. "The inadequate perfusion of the organs and tissues at rest or under load" in heart failure - is the result of open-AVA, which naturally leads to stasis capillary blood flow in some organs, perfusion to the slowdown.
2. Increased venous pressure in the vena cava and some veins of smaller caliber primarily because of the open ABA. Diseases of the heart valves and the venous valves are usually secondary.
3. "Apnea" occurs due to swelling of the lung tissue. Lungs not only have vessels of the pulmonary circulation, but also arteries and veins of the systemic circulation. At night, in a horizontal position, the excess venous pressure of a great circle reaches the lungs, because all human organs in the supine position are almost equal footing in relation to the Earth's gravity [3].
4. Reducing or maintaining ventricular ejection fraction of the heart, especially at the initial stage of development of heart failure, often does nothing. The problem of hypertension leads to dilation of the heart cavities. The statements regarding the impact of ejection fractions confirmed by the data published in the British Heart Foundation online magazine [10]. «Some people with heart failure have a normal ejection fraction, so ejection fraction is used alongside other tests to help diagnose heart failure». Additionally, there is information in the American Heart Association online journal [11]: «A significant proportion of patients with heart failure happen to have a normal ventricular ejection fraction at ECG during examination».
5. The occurrence and rate of development of heart failure is also influenced by additional human factors, including lifestyle, education level, physical activity, sedentary work, proper diet, special exercises, and genetics.
6. Apparently, there is found the explanation high values pairwise correlations between most of cardiovascular disease. Cardiovascular diseases are correlated with the some types of cancer. The reason is the "wrong" working AVA, it is in the position "open" too long and, unfortunately, are deep inside the human body.
Conclusions.
In my opinion, it is necessary to correct the errors in the field of cardiology. These errors have affected the efficiency of Cardiology for 50-100 years. It is necessary to check and discuss new proposals enabling a new era in cardiology.
References:
1. Ðаучный центр Ñердечно-ÑоÑудиÑтой хирургии им. Ð.Ð. Бакулева. Интернет реÑурÑ. 2017. http://www.bakulev.ru/cyclo/detail.php?ID=39219
2. Ermoshkin VI. New theory of arrhythmia. Conceptual substantiation of arrhythmia mechanisms. Cardiometry; Issue 8; May 2016; p.6–17; doi:10.12710/cardiometry.2016.8.617. http://www.cardiometry.net/issues/no8-may-2016/new-theory-of-arrhythmia
3. Ermoshkin VI. The mechanism of bronchial asthma. Why do the most serious asthma attacks occur at night? EC Cardiology, Volume 2 Issue 4 November 2016 https://www.ecronicon.com/eccy/pdf/ECCY-02-000030.pdf
4. Ermoshkin VI. Arteriovenous anastomoses and cardiovascular diseases. 8th Cardiovascular Nursing & Nurse Practitioners Meeting. August 08-09, 2016 Las Vegas, USA, DOI: 10.4172/2155-9880.C1.045 http://www.omicsonline.org/proceedings/arteriovenous-anastomoses-and-cardiovascular-diseases-48866.html
5. Ermoshkin VI. A New Theory of Certain Cardiovascular Diseases. EC Cardiology, Volume 2 Issue 5 November 2016 https://www.ecronicon.com/eccy/pdf/ECCY-02-000034.pdf
6. Ermoshkin VI. Venous congestion due to large arteriovenous anastomoses. 566 Chiswick High Road, London,
Greater London, W4 5YA, United Kingdom, DOI: 10.15761/HCCT.1000101 https://oatext.com/Venous-congestion-due-to-large-arteriovenous-anastomoses.php
7. Jyoty Malhotra, Paolo Boffetta. Association of increased cancer risk with heart failure. Journal of American College of Cardiology. Vol. 68, No 3, 2016.
8. Clark RA , Berry NM , Chowdhury MH , McCarthy AL , Ullah S. , Versace VL , Atherton JJ , Koczwara B , & Roder, D. (2016) Ð¡ÐµÑ€Ð´ÐµÑ‡Ð½Ð°Ñ Ð½ÐµÐ´Ð¾ÑтаточноÑÑ‚ÑŒ поÑле Ð»ÐµÑ‡ÐµÐ½Ð¸Ñ Ñ€Ð°ÐºÐ°: ХарактериÑтики, выживаемоÑти и ÑмертноÑти анализа данных , ÑвÑзанного Ñо здоровьем. Roder D. (2016) Heart failure following cancer treatment: Characteristics, survival and mortality of a linked health data analysis. Внутренние болезни журнал, 46 (11), ÑÑ‚Ñ€. 1297-1306. Internal Medicine Journal , 46 (11), pp. 1297-1306. http://eprints.qut.edu.au/101771/
9. Kamkin AG, Kiseleva IS, Yarygin VN. Fibrillation, defibrillation. Priroda. 2002;4:1040. [Russian]
10. British Heart Foundation. Heart failure. Internet resource. 2017. https://www.bhf.org.uk/heart-health/conditions/heart-failure
